This article outlines how the ADHD brain is wired differently to neurotypical brains, and discusses the risks of untreated ADHD.
Jump to section:
Introduction
ADHD-affected brains differ in both structure and function, and the most affected brain regions include the frontal lobe, prefrontal cortex (PFC), basal ganglia, limbic system, corpus callosum, and the default mode network (DMN) (see Figures 1 and 2 below). The neurotransmitters in a starring role here are dopamine and norepinephrine (Robins, 2023). In this article, the first of a two-part series, we look at both – starting with the neuroanatomy.
Editor’s note: This article focuses on the differences between ADHD and neurotypical brains, later highlighting the risks associated with untreated ADHD. In our next article (Harnessing ADHD Benefits with a Neurodivergent-affirmative Approach), we explore the same topic through a neurodivergent-affirmative perspective, focusing on the potential benefits of ADHD. For an introduction to the topic of neurodiversity, read this article (the first of a 3-part series). To learn more about ADHD’s types, symptoms and diagnostic criteria, read this article.
ADHD Neuroanatomy
The frontal lobe
This, the largest of the brain lobes, located at the front of the brain and the star player in the “executive control network,” is the most recent part of the brain to develop in humankind’s history, and is responsible for the ability to focus, plan, and remember things for more than a few seconds (see Figure 1). It is in the prefrontal cortex that we problem-solve, make decisions, control impulses, and utilise logic. Motivation resides here.
What is different in ADHD: The parts of the prefrontal cortex that manage attention and executive function are thinner in ADHD brains than they are in neurotypical brains. Parts of the prefrontal cortex can be underdeveloped in people with ADHD, causing deficiencies in executive functions such as working memory and the ability to plan and stay organised.
The basal ganglia
This part in the centre of our brain forms connections so that the different brain regions can work together (see Figure 1 below).
What is different in ADHD: For people with ADHD, there is less grey matter in the basal ganglia than in neurotypical people, although this apparently fills in with age. Thus, the traditional hyperactive-impulsive symptoms of some children are less pronounced by the time they become adults, even when those adults still meet the criteria for ADHD diagnosis.
The limbic system
Located mid-brain between the cerebral cortex and the brainstem, this collection of structures manages emotional responses and core survival behaviours.
What is different in ADHD: There is diminished white matter integrity in people with ADHD. White matter is a part of the limbic system that helps with learning, memory, and regulating emotions.
The corpus callosum
This part is also called “white matter”. It is primarily thought of as the communication network between the left and right hemispheres of the brain (see Figure 1).
What is different in ADHD: Those with ADHD have structural abnormalities in the white matter part of their brain. The abnormalities appear to be present even for those adults who believe that they have “outgrown” their ADHD (as approximately 25% of children with ADHD are believed to eventually do) (Robins, 2023).
The default mode network, or DMN
This special network, active when the mind is at rest (or in “default” mode), assists us in generating daydreams, self-referential thoughts, and those inward-looking thoughts. Because the DMN is a relatively recent concept, there is not complete scientific consensus on exactly which parts of the brain are involved in it. Nevertheless, structures that are generally considered part of the DMN include the medial prefrontal cortex, posterior cingulate cortex, and the inferior parietal lobule. The middle temporal lobe and the precuneus may also be involved (Neuroscientifically Challenged, 2023).
Activated when we are not working on external tasks or responding to external stimuli, the DMN is not typically active during tasks that require focus, problem-solving, or goal-directed thinking. In neurotypical people, it seems to work complementarily with areas such as the PFC (see Figure 2).
What is different in ADHD: People with ADHD are challenged to “turn off” the medial frontal cortex when they are performing a task that involves working memory. Hallowell and Ratey (2021) describe the ADHD brain as being like a popcorn machine that keeps shooting out pieces of popcorn, even if the owner of the machine doesn’t wish for that to keep happening!
The medial prefrontal cortex is part of the DMN network. Thus, with ADHD, the parts of the brain responsible for sustaining engagement with active cognitive tasks (i.e., those requiring planning, organising and decision-making) are in competition with the person’s DMN rather than working complementarily to it. So, for the person with ADHD, it’s extremely difficult to stop daydreaming when trying to focus on an important task; the DMN is just “in there” being active when it is meant to not be activating (Robins, 2023).
Figure 1: Parts of the brain affected by ADHD
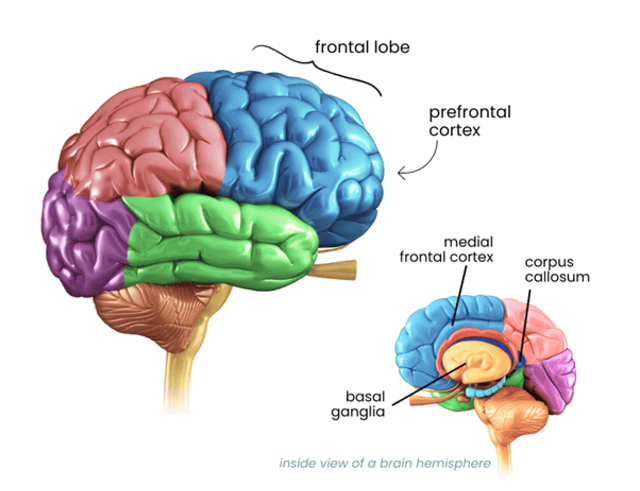
Image sourced from Inflow (Robins, 2023)
Figure 2: Parts of the brain involved in the default mode network (DMN)
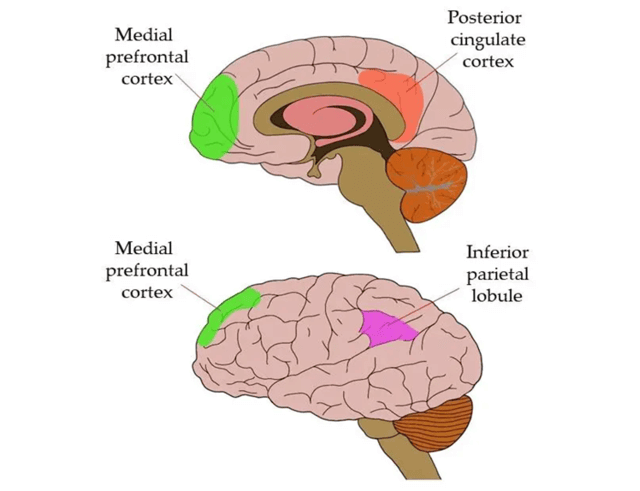
(Neuroscientifically Challenged, 2023)
The neurotransmitters that work differently in ADHD
It’s not just the brain’s structures, or anatomy, that we need to be aware of in the quest to understand the neurodiverse brain. We also have to deal with the neurotransmitters, the chemical messengers that help the nervous system send messages to and from nerve cells and neurons. In ADHD there are two standouts: dopamine and norepinephrine (a.k.a. noradrenalin).
Dopamine
This neurotransmitter has a primary role in transmitting messages of reward and pleasure. It is often characterised as the “reward-seeking neurotransmitter”, so it is key to understanding motivation, as well as being involved in focus and planning. It has dopamine receptors, proteins which allow dopamine to attach to a target cell, and dopamine transporters, which stop dopamine from providing that reward or pleasure, and so constitute the endpoint for dopamine’s action in the brain.
Neurotypical brains generally have a balance of dopamine, its receptors, and its transporters. So, when dopamine is released as pleasurable events occur – such as in sex, eating a favourite food, or receiving praise – we have enough receptors and transporters to complete the process normally.
What is different in ADHD: Researchers hypothesise a disruption in dopamine pathways with ADHD, which could happen in several ways. First, those with ADHD may have more dopamine transporters than neurotypical people, which could mean that excess dopamine molecules are removed from their brains, resulting in such individuals feeling less pleasure or reward from activities that neurotypical people enjoy. Low dopamine levels could also explain why people with ADHD are more at risk for engaging in dangerous behaviours, such as substance misuse, gambling, compulsive shopping, or risky sex. With low dopamine, they are seeking the rewards that neurotypical others would not have to engage in such extremes to enjoy.
Second, ADHD appears to be linked to an abnormality in the dopamine receptor gene, so those with ADHD have fewer dopamine receptors. With insufficient receptors, the brain can’t use all the dopamine that it does produce (Robins, 2023).
Norepinephrine/noradrenalin
Norepinephrine is both a neurotransmitter and hormone, As a neurotransmitter, it helps transmit nerve signals across nerve endings to another nerve cell, muscle cell, or gland cell. It also functions as a hormone, being released by a person’s adrenal grands (which sit atop each kidney). It’s made from dopamine, from nerve cells in the brainstem area of the brain and in an area near the spinal cord. Norepinephrine is part of the sympathetic nervous system, the body’s “fight or flight” emergency response system to danger, so it increases alertness, arousal, and attention, constricts blood vessels (to help maintain blood pressure in times of stress), and affects the sleep-wake cycle, mood, and memory (Cleveland Clinic, 2022).
What is different in ADHD: People with ADHD can have variants in the norepinephrine transporter gene, giving rise to behaviour problems and poor attention in children (Robins, 2023).
The risks of untreated ADHD
Adopting a non-pathologising, neurodivergent-affirmative approach when working with ADHD (the topic of our next article) presents numerous benefits. Likewise, it’s important to understand and acknowledge that ADHD also has a dark side; and seek appropriate treatment solutions.
Those diagnosed with ADHD as adults are more than four times likely to die prematurely than those not suffering from ADHD (Dimitriu, 2021). Here is why.
Distraction and the life-decreasing accidents
Smoking, obesity, and diabetes are diseases that shorten a person’s life expectancy. Recently Hallowell and Ratey (2021) quoted ADHD expert Russell Barkley as asserting that most people with ADHD (about 2/3) have a life expectancy reduced by up to 21 years: a much greater reduction than what we would expect to see from those other conditions. With ADHD, there is the tendency to become distracted, adventurous, and willing to engage in high-risk behaviours. Adolescents and young adults with ADHD have, according to a Journal of the American Medical Association (Pediatrics) article, a 36% higher incidence of motor vehicle crashes than their non-ADHD counterparts, regardless of age, sex, or driver licensure (Curry et al, 2017).
The internal and external distractions of ADHD lead to “attention failures”, which significantly increase the chances for causing a motor vehicle accident (Dimitriu, 2021). Sadly, this increased risk carries throughout the life span, and is even greater for those with co-morbidities such as anxiety and depression (Brunkhorst-Kanaan et al, 2021). Similarly, children and young adults with ADHD are said to be at greater risk of incurring fractures, burns, and poisonings, according to a study published in the Wiley Online Library (Prasad, West, Sayal, and Kendrick, 2018).
The addictions
We noted earlier how the somewhat dysfunctional executive function (pre-frontal cortex) of the ADHD brain, in conjunction with lowered levels of some neurotransmitters, such as dopamine, puts people with ADHD at much higher risk for developing substance misuse (related reading: Assessing and Treating Substance Abuse) or behavioural addictions (for a deep-dive on this topic, see MHA’s Working with Behavioural Addictionscredential course). In an assessment of about 12,000 children, the Lifespan Brain Institute of Children’s Hospital of Philadelphia and the University of Pennsylvania found that those not receiving treatment for their ADHD, but who were manifesting severe externalising behaviours, were more likely to express suicidal tendencies at one-year follow-up. This is of clear concern given that suicide is the second leading cause of death among those between the ages of 10 and 24 (CHOP, 2021). The study did go on to note, more positively, that appropriate ADHD medication could function as both a method for improving behavior and learning problems and a strategy for decreasing risk of suicide (Dimitriu, 2021).
What about parents who have ADHD?
Do parents with ADHD fail to recognise injury risk, or feel unable to enforce safety rules, thereby endangering their child? Some parents with ADHD may, through their lack of regard for their own safety, fail to see potential risks for their children and thus provide inadequate supervision, resulting in child injury.
The journal Medicine published an article which showed that this may be the case. The authors studied 40 children who had been admitted to hospital because of home injuries; the control group was comprised of 40 children who had been admitted for mild throat infections. The parents completed questionnaires assessing child behaviours, parenting attitudes, and whether they (the parents) had ADHD. The children who had been admitted for injuries had significantly higher scores for both internalising disorders (e.g., anxiety, depression) and externalising disorders (such as inattention or hyperactivity). And ADHD symptoms were significantly higher among fathers of injured children compared with the father of the 40 children admitted for throat infections. The authors concluded that psychopathology of parents is an important factor in children’s injuries (Acar, et al, 2015).
It’s not just the risk: Sub-optimal decision-making
Recall how one of the characteristics of ADHD is reduced capacity for executive function, meaning the organising, planning, and decision-making that goes with pre-frontal cortex action. Unfortunately, sub-optimal judgments and decisions are linked to ADHD through this. Thus, clients with ADHD have typically experienced motivational and other difficulties in putting in the necessary effort to make the best long-term decisions, says Dr. Alex Dimitriu, citing 2021 research from the Journal of Attention Disorders (Dimitriu, 2021).
ADHD courses and training
With ADHD being one of the most common neurodevelopmental disorders, it is crucial for therapists to be well-trained in its nuances. Following are some ADHD courses and training that you may be interested in:
- Working with ADHD in Children and Adolescents
- Working with ADHD in Adults
- OnTrac: A CBT Based Manualised Group Program for Adolescents with ADHD
Note: These courses are accessible (on-demand) through Mental Health Academy membership. If you are not currently a member, click here to learn more and join.
Key Takeaways
- ADHD-affected brains differ in both structure and function from neurotypical brains, and the most affected brain regions include the frontal lobe, prefrontal cortex (PFC), basal ganglia, limbic system, corpus callosum, and the default mode network.
- ADHD brains have disruption in dopamine pathways, resulting in less available dopamine to the person (so less pleasure and reward), and variants in the norepinephrine transporter gene (giving rise to behaviour problems).
- Adopting a neurodivergent-affirmative approach when working with ADHD presents numerous benefits. Likewise, it’s important to understand and acknowledge ADHD’s associated risks, and seek appropriate treatment solutions.
- People with ADHD may die prematurely due to distractions and accidents, higher incidence of addictions and risky behaviour, having an ADHD parent who supervises poorly, or making sub-optimal long-term decisions.
References
- Acar E, Dursun OB, Esin İS, Öğütlü H, Özcan H, Mutlu M. (2015). Unintentional Injuries in Preschool Age Children: Is There a Correlation With Parenting Style and Parental Attention Deficit and Hyperactivity Symptoms. Medicine (Baltimore). 2015 Aug;94(32): e1378. doi: 10.1097/MD.0000000000001378. PMID: 26266395; PMCID: PMC4616671.
- CHOP. (2021). ADHD medications associated with reduced risk of suicidality in children with significant behavioral symptoms. Children’s Hospital of Pennsylvania News. Retrieved on 5 June, 2023, from: https://www.chop.edu/news/adhd-medications-associated-reduced-risk-suicidality-children-significant-behavioral-symptoms
- Cleveland Clinic. (2022). Norepinephrine (noradrenalin). Cleveland Clinic. Retrieved on 4 June, 2023, from: https://my.clevelandclinic.org/health/articles/22610-norepinephrine-noradrenaline
- Curry AE, Metzger KB, Pfeiffer MR, Elliott MR, Winston FK, Power TJ. Motor Vehicle Crash Risk Among Adolescents and Young Adults with Attention-Deficit/Hyperactivity Disorder. JAMA (Journal of the American Medical Association) Pediatr. 2017;171(8):756–763. doi:10.1001/jamapediatrics.2017.0910
- Dimitriu, A. (2021). ADHD is not just lack of focus: The effects can be dangerous. Psychology Today. Retrieved on 5 June, 2023, from: https://www.psychologytoday.com/us/blog/psychiatry-and-sleep/202110/adhd-is-not-just-lack-focus-the-effects-can-be-dangerous
- Hallowell, E., & Ratey, J. J. (2021). ADHD 2.0. New York: Ballantine Books (an imprint of Random House).
- Neuroscientifically Challenged. (2023). Know your brain: Default mode network Neuroscientifically challenged. Retrieved on 4 June, 2023, from: https://neuroscientificallychallenged.com/posts/know-your-brain-default-mode-network
- Prasad, V.; West, J.; Sayal, K., Kendrick, D. (2018). Injury among children and young people with and without attention-deficit hyperactivity disorder in the community: The risk of fractures, thermal injuries, and poisonings. Child: Care, Health, and Development. Retrieved on 5 June, 2023, from: https://onlinelibrary.wiley.com/doi/10.1111/cch.12591
- Robins, B. (2023). Wired differently – the neuroscience of how ADHD affects the brain. Inflow. Retrieved on 1 June, 2023, from: https://www.getinflow.io/post/adhd-brain-science





